How we sleep may trigger or protect our brain from neurodegenerative disorders


According to recent mouse research, our sleeping posture may alter the glymphatic system, thereby increasing the chance of acquiring Amyotrophic Lateral Sclerosis (ALS) or other neurodegenerative disorders.
Furthermore, older persons diagnosed with Parkinson’s are likely to begin having awful dreams and nightmares a few years before exhibiting the disease’s hallmark characteristics, such as tremors, stiffness, and slow movement. In contrast, our dreams may disclose crucial information about the structure and function of our brains, making them an interesting focus for a neuroscience study.
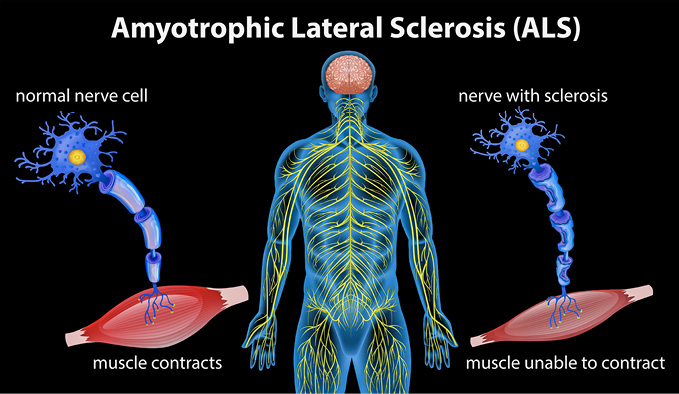
The most frequent motor neuron illness is ALS, which is Lou Gehrig’s disease. People who have ALS gradually lose the capacity to initiate and regulate muscular movements, including the ability to talk, swallow and breathe.
There is no recognised treatment. However, mouse research has found a new target in the battle against this deadly disease: the brain’s waste disposal mechanism. Neurodegenerative illnesses, such as Parkinson’s, Alzheimer’s and multiple sclerosis, have many commonalities, even though their clinical symptoms and disease development may seem significantly different.
The prevalence of these disorders rises with age. They are persistent and progressive, resulting in the slow loss of brain tissue. Waste proteins are also accumulated in the brain.
Protein chains, folds and misfolds
Long protein chains fold within our bodies to generate functional forms that enable them to execute specialised activities such as generating antibodies to combat infection, supporting cells, or transporting substances. This process may sometimes go wrong, resulting in “misfolded” proteins that cluster together to form aggregates. Misfolded proteins can expand and break, forming seeds that spread throughout the brain and create new clusters.
The build-up of waste proteins starts early in the neurodegenerative disease process, long before symptoms and brain loss appear. We wanted to explore whether removing or reducing the distribution of these waste proteins and their seeds may prevent or decrease disease development. The glymphatic (glial-lymphatic) system eliminates waste from the brain, including harmful proteins.
While humans are awake, this brain-wide network of fluid-filled spaces known as Virchow-Robin spaces is essentially turned off. However, it activates during sleep to transport substances necessary for brain function and to eliminate hazardous waste.
This might explain why all organisms, large and small (even flies), need sleep to thrive. (whales and dolphins, interestingly, rotate their sleep across brain hemispheres, keeping the other hemisphere awake to look for predators and signalling them to breathe!)
Sleep quality deteriorates as we age, and the risk of neurological diseases such as ALS rises. Sleep problems are another prevalent symptom of ALS, and studies have shown that even one night without sleep may increase toxic waste protein build-up in the brain.
As a result, we hypothesised that glymphatic function would be compromised in ALS. Researchers turned to mice to study this. The rodents were genetically altered to express human TDP-43, a protein linked to ALS. They were able to switch down TDP-43 protein expression in these animals by providing them antibiotic-containing chow (doxycycline).
 When the mice are fed a regular diet, the TDP-43 expression increases and misfolded proteins accumulate. The mice develop the hallmark symptoms of ALS, such as increasing muscular weakness and brain atrophy, over time. Researchers studied glymphatic function in these animals three weeks after turning on TDP-43 expression using magnetic resonance imaging (MRI).
When the mice are fed a regular diet, the TDP-43 expression increases and misfolded proteins accumulate. The mice develop the hallmark symptoms of ALS, such as increasing muscular weakness and brain atrophy, over time. Researchers studied glymphatic function in these animals three weeks after turning on TDP-43 expression using magnetic resonance imaging (MRI).
As they saw the glymphatic system at work, they discovered that TDP-43 animals exhibited lower glymphatic clearance than unmodified control mice. These variations were seen relatively early in the illness process, which is significant. As a result, the glymphatic system may be a promising therapeutic target in treating ALS.
How can we improve glymphatic function
Not all sleep is created equal. Sleep is divided into rapid eye movement (REM) sleep and non-REM sleep. Slow-wave sleep is included in this stage, when the glymphatic system is most active.
 Sleep medications that improve this period may be very effective in avoiding disorders like ALS. Glymphatic clearance is also known to be affected by sleep position. Glymphatic clearance is most effective in the lateral (or side-sleeping) posture, as opposed to the supine (on the back) or prone (front-lying) positions, according to mouse research.
Sleep medications that improve this period may be very effective in avoiding disorders like ALS. Glymphatic clearance is also known to be affected by sleep position. Glymphatic clearance is most effective in the lateral (or side-sleeping) posture, as opposed to the supine (on the back) or prone (front-lying) positions, according to mouse research.
The causes for this are unknown, however, they may be related to the effects of gravity, compression, and tissue stretching. Lifestyle decisions may also aid in the improvement of glymphatic function. Omega-3 fatty acids, present in marine fish, have long been thought to be helpful to health and lessen the risk of neurological illnesses.
According to a new study, these advantages may be partly attributable to Omega-3’s beneficial influence on lymphatic function. Short-term and long-term exposure to tiny quantities of alcohol was demonstrated in mice experiments to improve glymphatic function, however, excessive dosages had the reverse impact. Exercise has also been shown to be advantageous.
All of this research suggests that simple adjustments in lifestyle may increase brain waste elimination and reduce the risk of neurodegenerative illness. Following that, research should concentrate on medicines targeting the glymphatic system to aid people suffering from these terrible disorders.
Now, do you think position matters? – The Health
Dr Wael MY Mohamed is with the Department of Basic Medical Science, Kulliyyah of Medicine, International Islamic University Malaysia (IIUM).








