Factors that affect adolescents’ health are multifactorial and must be addressed holistically at all levels
Malaysia must invest in adolescent health programmes and development. It includes preventive, promotive, curative and rehabilitative care, delivered through smart partnerships with various stakeholders involving multidisciplinary teams.
Neglecting adolescent health will further contribute to the increasing disease burden in adulthood. Preventive interventions during adolescence are cost-effective in reducing morbidities and mortalities in adulthood, subsequently reducing the cost of treatment for NCDs among adults.

Director-General of Health, Datuk Dr Radzi Abu Hassan, said while young people were relatively healthy, there may be specific morbidities resulting from risky behaviours due to the very nature of the adolescent phase marked by dramatic hormonal changes.
“Evidence from the Lancet Commission (2016) has shown that investment in adolescent health is critical and provides triple dividend in ensuring the health of; current adolescents, in adulthood and future generations,” he told The Health.
By World Health Organisation (WHO) definition, an adolescent is 10-19 years.
Dr Radzi said factors affecting adolescents’ health are multifactorial and must therefore be addressed holistically at all levels (national, state, district and community) to identify their real needs.
“Their optimal growth and development are moulded in a supportive environment to produce healthy, knowledgeable, resilient and responsible adults.
Given the opportunity, adolescents and young adults are potent agents of change.
There is a need to enhance youth engagement to survive, thrive, and transform the world into a better place for future generations.”

“The investment should include adequate financial investment, provision of sufficient manpower and facilities. It is crucial to reduce the risky behaviours and enhance the protective factors that play an important role in the adolescents’ health.”
The National Health & Morbidity Survey (NHMS) 2022: Adolescent Health Survey (AHS) study assesses the health risk behaviours and protective factors among adolescents in Malaysia and reveals several significant findings.
The National Institutes of Health’s (NIH), Institute of Public Health (IKU) Director, Dr Noor Ani Ahmad, said: “Comparatively to our neighbouring countries, which also implemented Global School-based Student Health Survey (GSHS) using similar questionnaire and methods, our prevalence of health risk behaviours is among the highest in the region.”
The biggest concerns
NHMS 2022: AHS revealed that; obesity, attempting suicide, sedentary activity, current sexual intercourse, and current E-cigarette use showed increment trends of health risk behaviours. While the other health risk behaviours, such as alcoholism, drug use, and physical aggression, showed a slight decrease, the prevalence is still high.
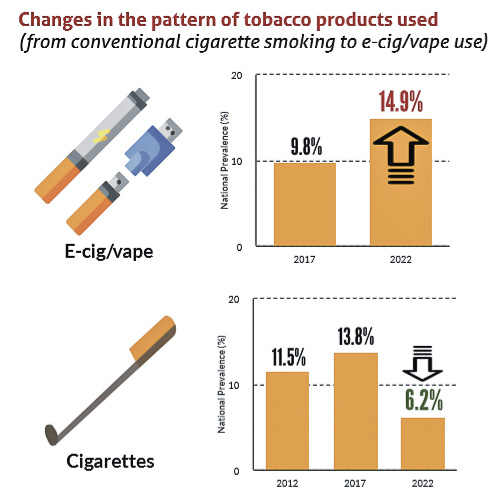
The prevalence of current cigarette smokers in 2022 (6.2 per cent) revealed a significant decrease compared to 2017 (13.8 per cent) & 2012 (11.5 per cent). However, there was a considerable increase in the prevalence of current E-cigarette/vape users in 2022 (14.9 per cent) compared to 2017 (9.8 per cent).
Second, regarding mental health problems, 26.9 per cent of adolescents reported being depressed. The trend of suicidal ideation among adolescents in Malaysia increased from 7.9 per cent in Malaysia in 2012 to 10.0 per cent in 2017 and 13.1 per cent in this current survey.
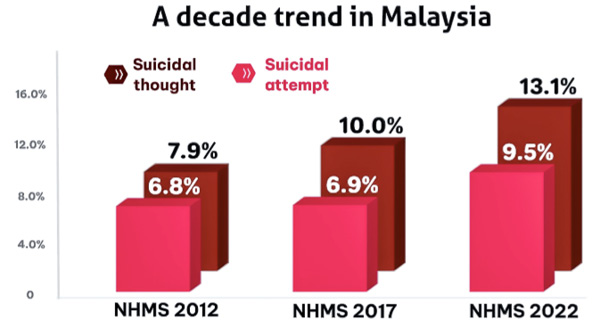
The prevalence of suicidal plans in this survey was also higher (10 per cent) compared to in 2012 (6.4 per cent) and 2017 (7.3 per cent). In addition, the suicide attempts were higher (9.5 per cent) compared to in 2012 (6.8 per cent) and 2017 (6.9 per cent).
Third, regarding nutritional status, the prevalence of underweight reported in this study was 8.3 per cent, which increased compared to seven per cent in 2012 and 6.5 per cent in 2017.
Addressing adolescent health problems

Given the NHMS 2022: AHS findings, Dr Noor Ani said the IKU suggested several recommendations. They include:
- Strengthening the multi-approach school-based nutrition and physical activity intervention to motivate behaviour modification to improve adolescents’ healthy eating and lifestyle.
- Improving the national school curriculum that teaches life skills such as effective coping strategies as part of “Program Minda Sihat”.
- More comprehensive sexual and reproductive health education programmes should be planned and executed among adolescents.
- Strengthening the current law and taking legal action in controlling the accessibility of tobacco products.
Commenting on the NHMS 2022, Dr Radzi acknowledged that the diversity of adolescents’ health problems must be addressed by all agencies/ stakeholders at the micro-level (individual, family, community) and macro-level (law/policymakers).
“MoH works in smart partnership through a whole-of-government approach with relevant ministries, agencies and institutions to provide health information, health education and healthcare services to adolescents in various settings via health clinics, schools, and community.
“It is pivotal to go beyond the health sector and develop strong multisectoral, whole-of-government policy approaches that truly address adolescent health and wellbeing.”
While the health sector may lead the overall response to health, addressing broad determinants of adolescent health and wellbeing requires multisectoral action, the most important of these is the education sector.
Additionally, Dr Radzi pointed out that Malaysia had developed a National Adolescent Health Policy and Plan of Action consisting of inputs from various government and non-government agencies involved in adolescent programmes and inputs from young people themselves.
“It is implemented through inter-sectoral collaborations in providing services targeting the wellbeing of adolescents and continuously advocating and creating awareness. The need for a national comprehensive intervention to tackle social determinants in all settings, at all levels and in all target groups is crucial.”
However, the remaining challenges must be sufficiently addressed in the policy regarding adolescent participation and access to information and services.
Based on the AHS and the Malaysian Population and Family Survey, knowledge of sexual and reproductive health (SRH) among adolescents is still low, and the prevalence of specific morbidities is increasing.
While children and adolescents have the right to access information and services, service providers still face challenges in dealing with children under 18 who are involved in risky behaviours and refuse to inform their parents, whereas being minors requires parental consent. Complex and sensitive issues related to sexual and reproductive health include requests for contraceptive information/ counselling and services and screening and treatment for STIs.
Dr Radzi noted gaps in policies and legislation regarding providing information and services to minors without parental consent.
“A clear policy is needed regarding dealing with complex and sensitive issues and considers the challenges faced by service providers in dealing with minors so that they have access to necessary and appropriate information and services, in ensuring their safety, health and wellbeing.”
Vaccine hesitancy
Meanwhile, the NHMS 2022: Maternal and Child Health (MCH) reported the prevalence of vaccine hesitancy in Malaysia as five per cent, marking the first nationwide study conducted among the population. The prevalence of vaccine hesitancy among parents in 2022 is at 4.9 per cent. This study serves as a baseline for understanding the burden of vaccine hesitancy in Malaysia.
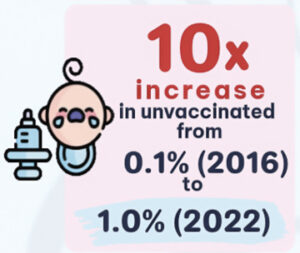
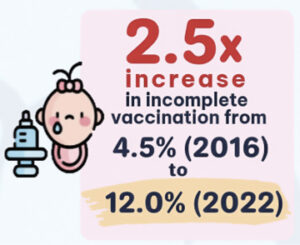 The Obstetrical and Gynaecological Society of Malaysia (OGSM) President-elect for 2022/2023 Prof Dr Nazimah Idris, said: “There is a huge increase in incomplete vaccination among children up to the age of 23 months from 4.5 per cent in 2016 to 12 per cent in 2022. Similarly, the percentage of unvaccinated children has increased 10-fold from 0.1 per cent in 2016 to one per cent in 2022. It is a very worrying trend indeed.
The Obstetrical and Gynaecological Society of Malaysia (OGSM) President-elect for 2022/2023 Prof Dr Nazimah Idris, said: “There is a huge increase in incomplete vaccination among children up to the age of 23 months from 4.5 per cent in 2016 to 12 per cent in 2022. Similarly, the percentage of unvaccinated children has increased 10-fold from 0.1 per cent in 2016 to one per cent in 2022. It is a very worrying trend indeed.
“Changing mindset is difficult because the reasons for vaccine hesitancy are usually not based on scientific arguments. Society needs to receive the correct information and have sufficient health literacy to make sense of the information and make good health decisions.

NHMS 2019, she shared, reported that one in three Malaysian adults had low health literacy.
“We must continue to educate and improve our health literacy and, at the same time, fight misinformation. If that is not enough, we should look into legislation, e.g., establishing an Act or regulation for all children (e.g. under five years) to be immunised.”
Dr Radzi stated that MoH Malaysia knew some parents were refusing or reluctant to vaccinate their children.
“The MoH’s Family Health Development Division has been monitoring the data closely for mothers who refused vaccinations from 2013. Among the reasons for refusals are concern about the halal status of vaccines, side effects and preference for using traditional or homoeopathy medicines.”
Therefore, the MoH and Immunise4life Programme have developed Modul “Menangani Ibubapa Yang Ragu atau Menolak Vaksin” mainly to deal with refused or hesitant parents.
The training was conducted in 2019 and 2020, with a second cycle of training, was carried out in 2022 involving all categories of staff involved in the National Immunisation Programme at the implementation level. – The Health