The cost of managing diabetes will continue to spiral to above RM5 billion per annum if Malaysians continue their love for sugar
It is estimated that one in five adults in Malaysia has diabetes. Yes, we are the sweetest nation in Asia, thanks to our love for everything sweet.

And if nothing is done, the cost, treatment and managing diabetes will continue to soar. Deputy Director of Health (Public Health) Datuk Dr Norhayati Rusli said: “This increasing trend poses a significant threat as diabetes is associated with many health complications. The Ministry of Health (MoH) spent approximately RM4.38 billion on managing diabetes in 2017.”
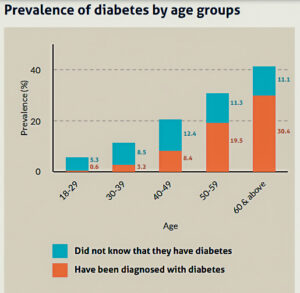
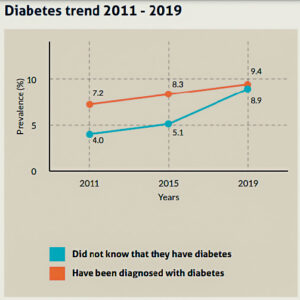
According to the 2019 National Health and Morbidity Survey (NHMS), Malaysian individuals 18 years of age and older are more likely than ever to have diabetes. The prevalence increased from 11.2 per cent in 2011 to 18.3 per cent in 2019, a 7.1 per cent rise.
Not only are the number of cases increasing, the cost of treatment is also high. Depending on the type and brand of insulin you require, the price in Malaysia can range from RM30 to RM200 each month or more. This does not include the cost of the shot administration equipment, blood sugar monitor, ongoing medical tests, constant medications and expensive long-term care.
According to President of the Federation of Malaysian Consumers Associations (FOMCA), Datuk Dr Marimuthu Nadason, the rising expense of diabetes will undoubtedly have a negative effect on patients in Malaysia.

“The estimated annual cost of diabetes in Malaysia is approximately US$600 million (RM2.6 billion). It is estimated that a person may spend between RM500 and RM1,000 per month in direct and indirect costs to manage the disease.
“It may make it more difficult to afford the necessary medications and medical care to manage their condition. This would undoubtedly lead to poorer health outcomes and an increased risk of complications from diabetes.
“Increasing treatment costs certainly put a severe financial strain on individuals and families already struggling with an increasing cost of living and low incomes.
“Especially for low-income patients but also for those in the lower levels of M40, this is a significant portion of their expenditure. Increasing costs may result in patients reducing their treatment for example, by reducing their supplements. This would certainly have a long-term impact on the patient’s health.”
Improving quality of managing diabetic patients
Said Dr Norhayati,“Diabetes is a specific chronic disease that needs to be managed comprehensively to prevent complications over time by a multidisciplinary care team.
 “Malaysia generally has an efficient and widespread system of health care, operating a two-tier health care system consisting of both a government-based universal healthcare system and a co-existing private healthcare system.
“Malaysia generally has an efficient and widespread system of health care, operating a two-tier health care system consisting of both a government-based universal healthcare system and a co-existing private healthcare system.
“The majority of people with diabetes seek treatment in public health facilities. Malaysia, through MoH, has established various programmes and interventions to ensure outstanding diabetes care is delivered.
“The establishment of Clinical Practice Guidelines Management of Type 2 Diabetes Mellitus (T2DM) provides evidence-based recommendations to assist healthcare providers in identifying, diagnosing and managing patients with T2DM.
“To support diabetes management in the primary care setting, yearly Diabetes Clinical Audit, together with the Enhanced Primary Health Care (EnPHC) initiative are in place to monitor the quality of management of diabetic patients, help to identify issues and improve further,” she added.
Type 1 diabetes (T1D) is an autoimmune condition where the body’s immune system mistakenly attacks and destroys cells in the pancreas that produce insulin, resulting in diabetes. This type of diabetes is more common in children and requires life-long insulin replacement to survive.
Type 2 diabetes (T2D) is caused by insulin resistance, where insulin is produced normally, but its function is impaired by excess body fat. In Malaysia, the prevalence of overall diabetes increased with age, from 5.4 per cent in the 20-24 age group, reaching a peak of 43.4 per cent (95 per cent CI: 37.37, 49.65) among the 65-69 years old as reported by NHMS 2019.

“Unfortunately, T2D is no longer a condition that only affects older people, although the likelihood does increase with age. It is now increasingly seen among adolescents with the rise of childhood obesity,” shared Dr Norhayati.

According to Duopharma Biotech Berhad CEO (Commercial), Wan Amir-Jeffery Wan Abdul Majid, there may be periodic price increases on drugs and medication due to input and supply chain costs.
“And in the last three years, it is evident that the costs in the supply chain, raw material, packaging and even logistics have increased significantly.”
Echoing Wan Amir-Jeffery, Malaysian Pharmacists Society (MPS) President Prof Amrahi Buang stated that the pandemic had contributed to price hikes due to border control, active pharmaceutical ingredient (API) supply disruption, and packaging material disruptions.

“The pandemic resulted in concerns of medicine security and an immense increase in the cost of drugs.”
Scaling up facilities and bringing down costs
In response to how to cope with the increase in diabetes-related cases, National Diabetes Institute (NADI) Chairman, Emeritus Prof Datuk Dr Mustaffa Embong, said: “There is a need to put in place adequate capacity in health services like more health clinics with adequate staffing including nurses and doctors.
“We should also create a dedicated body to monitor cardiometabolic diseases and provide advice on reversing the worsening trends.”

Meanwhile, Consultant Physician and Endocrinologist Dr Shalini Sree Dharan said: “We can create more diabetes one-stop centres that can support our patients with the help they need at a cheaper cost as insulin needles, glucometers and strips which are more affordable.
“Medications which have been proven effective in reducing diabetes-related complications should be reduced in price to make it more affordable to the majority.”
Parti Sosialis Malaysia (PSM) Chairman Dr Michael Jeyakumar agreed on the importance of scaling up the capacity of the nation’s healthcare system to deliver diabetes early intervention and comprehensive treatment.
“The government must put more funds into healthcare by raising it to four per cent of GDP from the current 2.3 per cent.

“Early interventions are important to save patients from suffering complications, which are often only partially reversible and lead to many morbidities. It affects their capacity to earn or look after their families, and the treatment they need is an additional expenditure for the country.”
He added: “Many government clinics have dedicated clinics for diabetes. These should be made available in more government outpatient departments (OPDs) and be staffed by dedicated nurses whose role should include educating these patients on diet, weight control, exercise, etc.”
Health literacy and awareness are key
Inadequate health literacy hinders people from understanding their health, seeking help, and protecting themselves from risk factors and illness.
“Lack of awareness from individuals and society for behaviour change to reduce risk of diabetes is also an important factor,” said Dr Norhayati.
“Data from our National Health and Morbidity Survey (NHMS) in 2019 showed that in general, 35.1 per cent of adults have low health literacy; 28 per cent have low health literacy in managing medical issues, 32.3 per cent have low health literacy related to disease prevention activities, while 27 per cent have low health literacy in health promotion and healthy lifestyle practices.
“Patients and caretakers need to understand and be knowledgeable about their condition and accept responsibility for self-care. We need a whole-of-society, and whole-of-government approach as health is the MoH’s and everyone’s responsibility.”
Meanwhile, Dr Jeyakumar suggested creating more awareness in the general public via drama series with a diabetic person as one of the key characters, which he believes would be much better and more effective than dry and boring lectures by doctors.

The Association of Specialists in Private Medical Practice in Malaysia (ASPMP) organises diabetes workshops and health screening camps annually to update doctors and the public about the early detection of diabetes and its early intervention.
Its President Datuk Dr Balwant Singh Gendeh, said this was done through its Physicians/Endocrinologists in collaboration with the Malaysian Medical Association (MMA).
So what can be done to persuade Malaysians to reduce their high intake of high sugar content products?
Said Marimuthu, ”To change consumer behaviour we need to change both the consumer’s environment and his behaviour. Environmental change, he explained, would include implementing taxes on sugary food and drinks, which would increase the price of these items, making them less appealing to consumers.

“Eliminating sugar subsidies and adding a sugar tax would reduce sugar consumption. Due to the extremely high level of diabetes in Malaysia, this may be painful but a necessary step in Malaysia.
“The government can also encourage the food industry to reduce sugar in their products and offer subsidies or other incentives to promote businesses to provide healthier food options, such as fruits and vegetables.
“Restricting advertising and marketing of sugary products to children. This can help prevent children from developing a taste for sugary food at a young age.”
He said: “Governments must also improve access to healthy food in low-income communities and make it more affordable.”
He also emphasised starting early and educating children on healthy diets and lifestyles. “Ensure affordable healthy foods at school canteens and collaborate with schools to promote healthy eating.” – The Health
A severe disease
Diabetes is a severe and chronic disease that occurs either when the pancreas does not create enough insulin or when the body cannot use the insulin produced.
A normal HbA1c test level is below 5.7 per cent. A level of 5.7 per cent to 6.4 per cent indicates prediabetes and a level of 6.5 per cent or more indicates diabetes. Within the 5.7 per cent to 6.4 per cent prediabetes range, the higher your HbA1c, the greater your risk is for developing Type 2 diabetes.
The prevalence of diabetes has been progressively rising over the past few decades. The World Health Organisation (WHO) Global Report on Diabetes states that in 2014, an estimated 422 million adults worldwide had diabetes, up from 108 million in 1980.
It is of concern that the number of diabetes cases is increasing, and the rising cost of treatment adds to the burden of the disease.
Diabetes and its complications result in significant economic losses for those with it, their families, health care systems, and national economies due to direct medical expenses and lost wages and income.
The International Diabetes Federation (IDF) estimates that between 2003 and 2013, the total amount spent globally on diabetes healthcare more than quadrupled as a result of both an increase in the number of individuals with the disease and an increase in per capita diabetes spending. – The Health