There needs to be greater synergy between the various healthcare stakeholders within the government, private sector and civil society groups

BY ROSHEL JAYASUNDERA
CONTINUOUS improvements within Malaysia’s healthcare ecosystem mean more people in the country now have better access to quality healthcare and are therefore living longer.
However, maintaining this quality is becoming a larger healthcare burden, testing the limits of healthcare system capacity in the longer term. Concurrently, more patients are opting to receive care outside of hospitals and clinics due to overcapacity issues and the fear of contracting Covid-19.
These issues pose a challenge for healthcare systems as ensuring continuity is important for generating positive healthcare outcomes. For instance, patients with critically fatal diseases such as cancer require specialised treatment, but many are often unable to access the medication they need in time – especially if they come from more vulnerable population groups.
Healthcare systems are then at risk of collapse as they cannot successfully address specific threats such as brain cancer. Although not currently one of the largest contributors to cancer cases in the country, they still often present a high incident-to-death ratio.
For Malaysia to build a more resolute and accessible healthcare future, there needs to be greater synergy between the various healthcare stakeholders within the government, the private sector and civil society groups. These players must work more closely together – particularly outside of purely clinical settings – to understand the real needs of patients and how to best tackle perennial issues across multiple dimensions such as access and affordability.
Multi-sectoral collaboration
Today, healthcare systems must go beyond the long-standing top-down models typically associated with state-provided healthcare. This is because healthcare needs in Malaysia are growing but so are its costs, placing more demand on government budgets.
Ultimately, this means the responsibility for treatment and other medical costs is increasingly falling on the patient, who must now take a more active role in treatment decisions – particularly those related to pursuing, paying for and staying on treatment outside of clinical settings.
Even so, broadening healthcare access is not a one-size-fits-all approach that happens only in clinical settings; it requires one that is personalised and tailored to the specific needs of the patient and their country. This is especially for specialty treatments in Malaysia, such as oncology treatment which may be too costly for patients and still lack universal coverage.
With more money needing to be paid out of the patient’s pockets, there can be a late presentation of the disease, leading to more expensive treatment and poorer outcomes.
This means that healthcare stakeholders outside government – including the private sector and civil society groups – are well-positioned to support the country’s broader healthcare system improvement efforts. However, they must venture outside of their siloes and work more closely to explore better ways for patients to adhere to their treatment regimens.
But before doing so, they must understand the various dimensions of factors that affect a patient’s healthcare decision-making.
Harnessing insights across dimensions
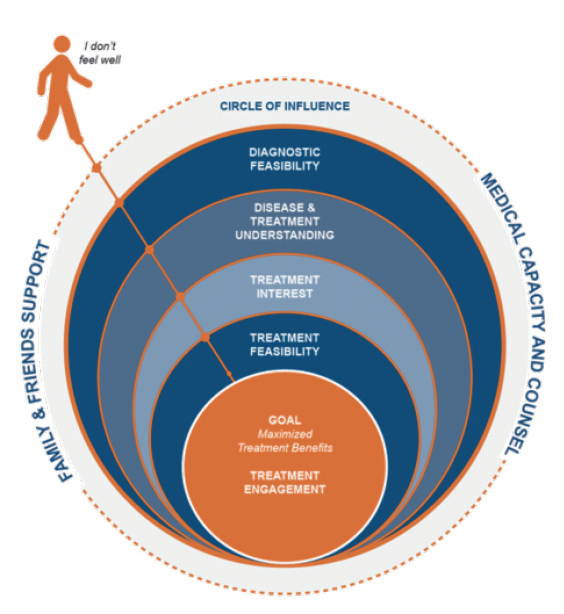
To improve the effectiveness of multi-sectoral approaches in addressing growing burdens such as cancer, they must first understand in detail how a complex set of factors guides a patient’s healthcare decisions. As these factors cut across multiple dimensions, the factors can be determined through a comprehensive assessment of the patient’s needs and affordability.
A complex set of considerations guides patient decisions (see Figure 1). These considerations can be measured to understand how specific patient requirements vary across treatment adherence dimensions, which then helps to inform customised adherence and support plans that maximise treatment benefits.
To ensure accuracy of these plans, there must also be a detailed assessment and understanding of the risk factors which may impact the patient’s adherence to treatment. A Patient Needs Assessment Tool (PNAT) facilitates this assessment, helping to understand better the patient’s unmet needs across the five dimensions of adherence proposed by the World Health Organisation (WHO). They are:
- Social and economic: i.e., patient’s socio-economic status; literacy and education levels; culture; age; and availability of social support
- Therapy-related: i.e., treatment regimen complexity; treatment duration; the immediacy of beneficial treatment effects; and side effects from treatment
- Patient-related: i.e., resource availability; knowledge; attitudes; motivation; expectations; and beliefs
- Healthcare team and system: healthcare coverage availability; relationships between patients and clinicians; and skill and training of clinicians
- Condition-related: symptom severity; disability levels; rate of disease progression; and comorbidities
After considering a patient’s unique needs, a Patient Financial Eligibility Tool (PFET) can assess how much assistance an individual patient needs to afford their full treatment course. This tool must measure three different indicators of a patient’s wealth – indicated by income, assets and living standards. These are then used to develop a plan that details how much of the treatment course a patient must pay based on their ability to pay.
The insights obtained from tools such as PNAT and PFET can then help inform multi-sectoral healthcare efforts. For instance, with more detailed information on hand, healthcare providers and ecosystem stakeholders can then develop cost-sharing models that help widen access to specialised medications – namely how much will be covered by other parties, such as pharmaceutical companies, insurers, and the government.
By splitting the cost of treatment across multiple parties, cost-sharing makes it possible for patients to afford their entire course of treatment. Patients then maximise their treatment’s medical benefits, whereas physicians have a viable alternative for patients experiencing access issues.
This can also help minimise demand on government healthcare budgets, while NGOs and civil society groups helping more vulnerable societal segments pay for treatment will have more clarity on how to raise and/or disburse financial support more accurately.
Multiplying efforts to transform patient outcomes in Malaysia
If its access needs remain unaddressed, Malaysia’s national healthcare system will be strained in its ability to adapt to the ever-evolving needs of patients in the country. We are already seeing healthcare transformation efforts being driven by the government and private sector to overcome existing access hurdles – particularly in terms of digitalisation.
However, multisectoral initiatives must reinforce such efforts that can accurately determine the multi-dimensional factors behind a patient’s access limitations. Doing so will help generate better health outcomes and scale it, thus raising the quality of healthcare access in Malaysia and sustaining it. — The Health
Roshel Jayasundera is Senior Director, Global Consulting at Axios International, a global healthcare access company







