Government funding will comprise most of the health fund’s budget, though future financing may come from large donors and private donations
 The Health White Paper for Malaysia (HWP) aims to address the challenges associated with healthcare financing, the rising cost of healthcare, and the sustainability of healthcare funding.
The Health White Paper for Malaysia (HWP) aims to address the challenges associated with healthcare financing, the rising cost of healthcare, and the sustainability of healthcare funding.
Ensuring Sustainable and Equitable Health Financing was pillar three of the health reform pillars and strategies mentioned in the HWP. The pillar includes significant systemic and structural improvements designed to make health financing more sustainable and value-driven while improving financial risk protection and reducing out-of-pocket expenses.
The HWP was presented in Parliament on June 15 by Health Minister Dr Zaliha Mustafa. It provided several recommendations on how to gradually increase investments in health, diversify the sources of funding for the sector, pool risks, and improve spending efficiency.
One of the reform strategies to ensure the population’s access to affordable, comprehensive services is the development and establishment of the health benefits package.
Establishing a benefit package for the population, financed by a dedicated health fund, will allow for greater pooling of health and financial risk within the population and greater cross-subsidisation for Universal Health Coverage.

The benefit package will provide a specified set of health services and medications at affordable fees with the same level of care, regardless the provider is from the public, private or non-profit sector.
“The benefit package will encompass a range of evidence-based services, including promotive and preventive services, from primary healthcare to hospital care, including potentially from digital health providers.
“The scope of the benefit package will be based on objective economic and health technology assessments and will continuously evolve as Malaysia’s health financing system matures and in response to changing health needs,” said the HWP.
A dedicated health fund to be established will pay for the services used by the population under the benefit package. Government funding will comprise most of the health fund’s budget, though future financing may come from large donors and private donations.
The fund will be managed by the not-for-profit professional Strategic Purchaser governed by clear reporting standards and robust regulatory oversight to ensure its administration doesn’t strain the public purse and serves the public interest.
Increasing investment in health
To achieve Universal Health Coverage and protect individuals from financial risk when they fall ill, the HWP also emphasised the need for publicly managed health funding from various sources, including the government, individuals, and companies needs to be gradually increased to five per cent of GDP.
This increment will also consider strategic collaboration and using resources and assets across various stakeholders.
“Given the increasing health needs from Malaysia’s changing demographics, relying on a single source to support the financing of public health is neither sustainable nor equitable. A form of social compact will be proposed which calls on to share the responsibility of investing in health.
“As part of this, options for progressive contributory schemes will be explored, deliberated and, if found suitable, presented to Parliament for bi-partisan acceptance.”
Other proposed initiatives include reviewing and revising fee structures at public sector healthcare facilities.
“The low fees charged by public healthcare facilities is a highly valued feature of the country’s health system, allowing affordable access to millions of users.
“Nevertheless, the one-size-fits-all fee structure has contributed to the immense disparity between fees charged against the cost of provision and the less-noted gap between the prices charged versus the capacity and willingness to pay, particularly amongst higher income households.
“To improve the sustainability of public healthcare funding, the range of fees and charges in public healthcare facilities will be reviewed to be more commensurate with different affordability levels while still maintaining the safety nets and current affordability levels for lower-income households.”
Who will manage the proposed health fund?
The HWP also stated that increasing the effectiveness and efficiency of healthcare spending is just as important as growing investments and funding when it comes to ensuring the sustainability of health financing.
New roles and strategic practices will be introduced to ensure that increased health investments significantly impact the nation’s health outcomes.
“A not-for-profit Strategic Purchaser will manage the proposed dedicated
health fund.
“The Strategic Purchaser will procure healthcare services from the public and private sector through innovative and value-based payment models that drive better outcomes, service coverage, cost-effectiveness, quality, and performance from providers. Clear reporting standards and robust regulatory oversight will also govern Strategic Purchaser.”
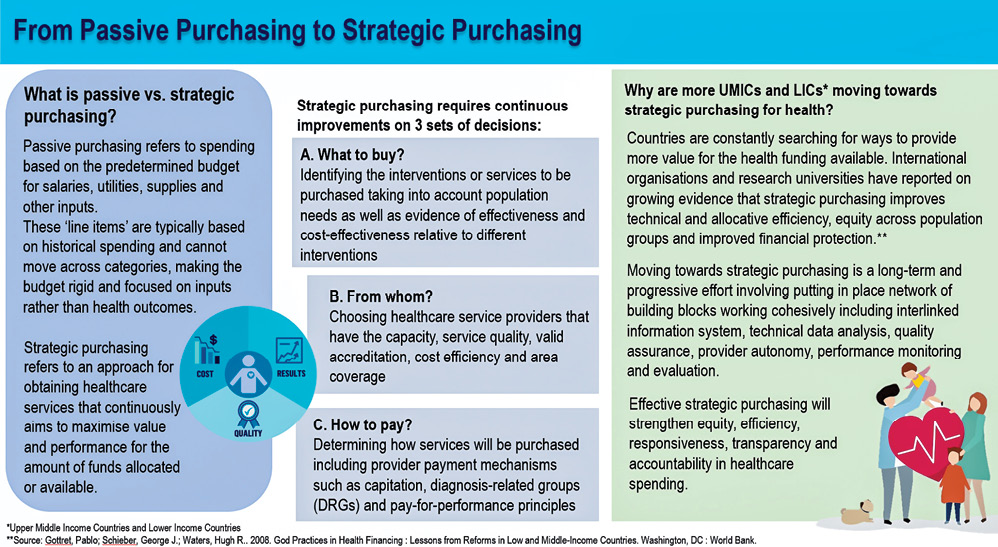
Effective health spending is also driven by allocative efficiency across different programs within the Ministry of Health (MoH) and relevant government agencies and ministries.
The HWP proposal to transform primary healthcare, strengthen public health functions and stimulate promotive and preventive approaches provides the direction towards better allocative efficiency within the health system.
Periodic reviews will assess whether funding to specific programs, units, departments, or divisions is adequate and well spent in achieving the desired outcomes.
Additionally, the HWP intends to scale up digitalisation and increase autonomy for public sector healthcare facilities, contributing to more significant operational and financial efficiencies.
“To reduce inefficiencies and wastages further, administrative processes and criteria will be reviewed and revised to reduce bureaucracy and improve responsiveness. Effective and responsible healthcare spending also means recognising the impact of healthcare energy consumption and consumables on planetary health and climate change.
“The MoH will reduce carbon emissions through increased use of renewable energy. The production of pollutants and non-biodegradable waste will be tackled through continuous improvements in medical waste management initiatives.
“Improving the effectiveness and cost-effectiveness of health spending will maximise every Ringgit invested into the system to produce continuous improvements in health outcomes amongst the population. The mindset of the health sector will also evolve to be more value-and performance-driven.”
The HWP stated the efforts to systematically and structurally improve the effectiveness of health spending are currently either at the early implementation stage or at the planning stage. – The Health
Four pillars to strengthen healthcare system
The 57-page Health White Paper (HWP) outlined the current status, gaps and constraints the country’s health system faces and proposed structural and systemic solutions that included reforms in service delivery, financing and governance over 15 years.
The short-term phase will commence in 2024, the medium-term phase will begin in 2029, and the long-term phase will run from 2034 to 2039.
 The HWP proposes four pillars and 15 strategies for strengthening the healthcare system. The pillars are:
The HWP proposes four pillars and 15 strategies for strengthening the healthcare system. The pillars are:
- Pillar 1: To transform the delivery of healthcare services in the country by prioritising and restructuring primary healthcare; optimising hospital care; granting operational autonomy to public sector providers and increasing partnership with private sector providers; and harnessing digitalisation and technology for overall service delivery improvement.
- Pillar 2: To cultivate and ground health promotion and disease prevention approaches at all levels in the nation by improving public health and health emergency preparedness functions; improving processes to drive shared ownership of health outcomes amongst government agencies; improving methods for coordination and collaboration with stakeholder groups in communities and society; and increasing the application of incentives and disincentives to acculturate healthy behaviours and norms.
- Pillar 3: To place the financing of the health system on a sustainable footing towards progressively increasing health funding under public sector management; exploring and implementing equitable ways of diversifying sources of health funding; pooling the population’s health risk into a dedicated health fund that ensures affordable coverage over a comprehensive set of services; and ensuring the cost-effectiveness of health expenditure by instituting a range of organisational and governance reforms including the establishment of value-based payment models and the strengthening of the Strategic Purchaser.
- Pillar 4: To strengthen the organisational, governance and stewardship foundations of the health system by strengthening the Ministry of Health’s (MoH) policy-making, regulatory, data stewardship and research functions; devolving the healthcare provider and purchaser role from the MoH to institute greater check-and-balance as well as performance; improving policies, legislation and regulations related to health to be relevant to the current situation; improving the health workforce ecosystem including planning, credentialing, career development, public sector recruitment and deployment; and stimulating research, innovation and evidence-based approaches.
Some of the reform themes contained in the pillars and strategies above gained increased prominence recently, but many others are familiar to Malaysia. Since the 1980s, multiple efforts have addressed the systemic challenges inherent in the country’s health system.
While many stakeholders have highlighted the clear need for systemic and structural shifts, long-term change has not been purposefully introduced due to the lack of clear agreement on the direction of reform.
Notably, the HWP was initiated by former Health Minister Khairy Jamaluddin back in January 2022 to reform the country’s health system, especially in ensuring that it is future-proof.
This critical component, namely securing broad agreement on the case for change and the path forward for Malaysia’s health system, is the purpose of presenting the HWP in Parliament.
The direction of the health system reform pillars proposed by the HWP is sufficiently broad and enduring; nevertheless, reform efforts need to be able to adapt and course-correct in the face of learnings, improved methods or models and new technologies.
In that regard, the strategies proposed may be refined during the HWP reform period upon the government’s recommendation, the health reform monitoring body or Parliamentary Select Committees, after debate and deliberation in Parliament.
Health system reform in Malaysia is necessary and urgent. Reform of the health system is required to prepare the system for the future, enable Malaysians to live in better health, and for the nation to prosper.
Before more time is lost, Parliament, the people and the nation must stand together and begin the journey of health system reform today. – The Health








